Everything You Need to Know About Psilocybin and Depression
A comprehensive guide to understanding the research on psilocybin for depression and the potential benefits of using psilocybin therapy to treat depression.
Published on: September 22, 2025
A Complete Overview of Psilocybin and Depression
Can psilocybin, the active component in magic mushrooms, offer legitimate, lasting relief for people struggling with depression?
Mounting research suggests the answer is a compelling yes.
In recent years, psychedelic mushrooms have shed their stigma as a dangerous drug or relic of counterculture. Psilocybin is now at the forefront of a mental health revolution, with clinical studies demonstrating its potential to help treat depression, especially in individuals who haven’t responded to conventional therapy such as SSRI medication (Mann, 2023).
When paired with psychotherapy and administered in a professionally guided setting, psilocybin offers new hope for those facing depression, leading to lasting changes in mood, perspective, and emotional well-being.
In this comprehensive guide, we’ll explore:
- What psilocybin is, and how it impacts the default mode network
- Understanding the different factors behind depression and how psilocybin can help
- How psilocybin works in the brain and how this supports long-lasting relief from depression
- The psychedelic effects of psilocybin experiences and how this can help depression
- The safety of psilocybin, and who psilocybin isn’t for
- The power of group retreats for psilocybin healing
- Why integration is key for long-term change in depression
- Psilocybin’s legal status and options for accessing it
Psilocybin is a New Hope For Depression
Living with depression can be profoundly debilitating, affecting every aspect of a person’s life – from self-care and personal goals to their ability to function at home, work, school, and maintain meaningful relationships.
Yet over 280 million people globally struggle with some form of depression, including 5% of adults, according to the World Health Organization. In the US alone, an estimated 21 million adults had one major depressive episode in 2021, representing 8.3% of all adults.
While emotional fluctuations and periods of feeling down are part of the normal human experience, depression, which is characterized by prolonged episodes of low mood that lead to disruption in a person’s life, often requires specialized treatment.
Depression can manifest in many ways, but typically involves persistent feelings of sadness or emptiness, a loss of meaning and pleasure, and a sense of hopelessness about the future.
While there are many options for people struggling with depression, it can be difficult and time-consuming to find the right treatment. People with depression are often recommended psychotherapy, which, while effective, isn’t a cure-all. Response rates hover at around 40-50% across therapies (Cuijpers et al., 2021), and it typically takes multiple sessions over several months to achieve benefits (Machado-Vieira et al., 2010).
Psychotherapy can help individuals gain a cognitive understanding of their challenges, acquire tools for symptom management, and assist them in beginning to process past traumas. However, for many cases, it can only take the person so far, and what they require is healing that takes place beyond the rational, conscious mind.
Antidepressant medications like serotonin reuptake inhibitors (SSRIs) can also help relieve depressive symptoms, but research indicates they are overprescribed and used for longer than is necessary (Brisnik et al., 2024).
Around 53% to 64% of people experience a significant reduction in symptoms while using SSRIs (Hirschfield, 1999), and they typically take 6-8 weeks to have a full therapeutic effect. Many patients report side effects, including continual nausea, sexual dysfunction, weight gain, sleep disturbances, and emotional blunting – yet around one in eight Americans use antidepressants.
What’s more, antidepressants don’t address the root cause of an individual’s depression. While they may alleviate symptoms, they typically don’t help individuals understand the psychological origins of their distress or begin the deeper process of emotional healing (Barton et al., 2024) and nervous system regulation to overcome depression.
Meanwhile, studies on psilocybin-assisted therapy show its potential to reduce depression symptoms drastically. One study on people living with major depressive disorder (MDD) found that mean depression scores rapidly decreased the day after the psilocybin session and remained low through the four-week follow-up, with 54% of patients in remission one month post-session (Davis et al., 2020).
Another study found that psilocybin-assisted therapy has comparable antidepressant effects to a six-week course of the popular SSRI, escitalopram (Carrhart-Harris et al., 2021). At the six-month mark, researchers found that the psilocybin group had experienced additional psychological benefits compared to the SSRI group, including psychological connectedness, finding meaning in life, and functioning well at work and in society (Erritzoe et al., 2024).
What is Psilocybin? A Brief Overview
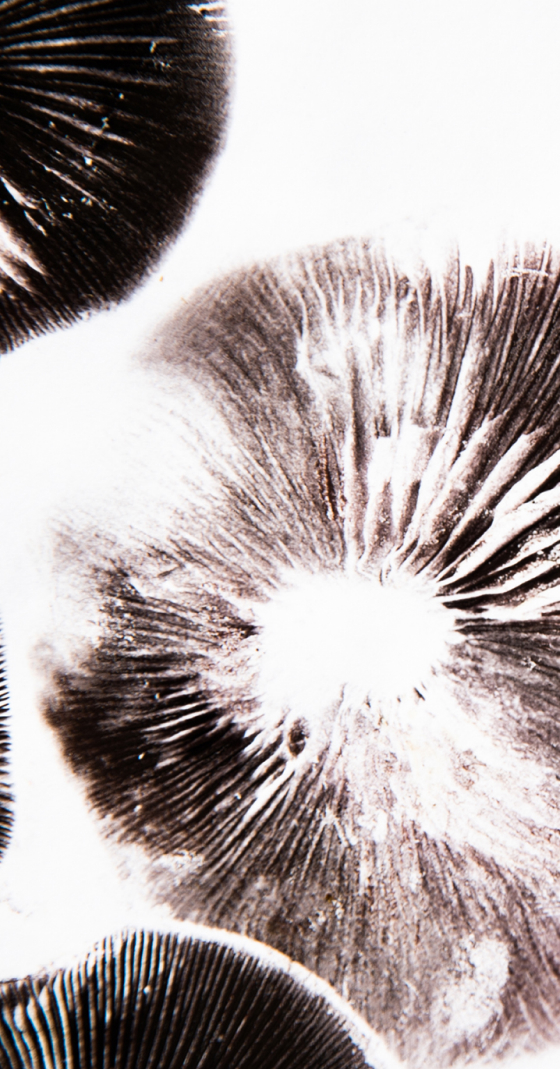
Ever heard of “magic mushrooms”? It turns out these psychedelic fungi have a powerful psychoactive compound that can promote profound healing in the body, brain, and mind. Psilocybin is found in over 180 species of mushrooms, with the most common ones being Psilocybe cubensis – also known by common strains such as “golden teachers.”
Psychedelic mushrooms have been used for thousands of years by Indigenous people worldwide (Spiers et al., 2024). In Mesoamerica, in particular, Native communities such as the Mazatec people used (and continue to use) psilocybin mushrooms in rituals, to connect with the spirit world, and treat physical ailments.
Psilocybin mushrooms were introduced to Western culture in the 1950s, when American banker R. Gordon Wasson traveled to Oaxaca, Mexico, to participate in a Mazatec psilocybin mushroom ceremony with Indigenous curandera Maria Sabina.
Wasson then wrote about his experiences in Life Magazine, which influenced the ensuing counterculture in the US and drove spiritual seekers to travel to Mexico in the 1960s in search of similar ceremonies.
However, the Controlled Substances Act of 1971 put a halt to much of the research into psilocybin and other psychedelics and marked the beginning of the War on Drugs.
After this decades-long freeze, psilocybin research saw an uptick in the early 2000s. Since then, researchers have been exploring the mechanisms, safety, and therapeutic potential of psilocybin, with study results indicating its potential to treat various mental health conditions.
How Psilocybin Impacts the Default Mode Network
Once ingested, psilocybin is rapidly metabolized in the liver into psilocin, which is the active compound responsible for the psychoactive effects of psilocybin mushrooms, i.e., the psychedelic experience.
Psilocin structurally resembles serotonin, a key neurotransmitter involved in mood regulation, cognition, and perception. Due to this similarity, psilocybin primarily binds to serotonin 5-HT2A receptors, particularly in areas of the brain associated with self-awareness, sensory processing, and emotional regulation.
All of this leads to temporary changes in brain network connectivity. This is especially the case in the Default Mode Network (DMN), which is the part of the brain that is involved with internal mental processes, such as rumination, recalling memories, or thinking about the future.
When the DMN is disrupted during a psilocybin experience, it is said that the ego quietens or, at higher doses, dissolves completely. This leads to users experiencing a sense of interconnectedness with others, the world around them, and new psychological aspects of themselves. The changes evoked by psilocybin within this highly complex brain network potentially play a key role in breaking the thought cycles that are common in depression.
We’ll delve deeper into these mechanisms and how they alleviate depressive symptoms later in the article.
Psilocybin Induces Altered States with Therapeutic Potential
So, what does all of this feel like when you’re under the influence of psilocybin?
When taken in a safe and supportive setting, psilocybin can open the mind to new experiences, facilitate deep emotional breakthroughs, and increase psychological flexibility. Users report profound changes in their perceptions (i.e., visions, thought processes, emotional fluidity), as well as mystical and transpersonal experiences, such as feeling “at one” with the universe and/or the natural world.
At this point, it’s important to distinguish between therapeutic and recreational use. When taken recreationally or without the proper set and setting (i.e., going into the experience with a prepared mindset and in a safe and supportive setting for deep personal exploration), psilocybin carries risks.
Without a safe, well-thought-out set and setting, people can come out of the experience feeling psychologically destabilized. They may also be vulnerable to various types of harm while under the influence of the psychedelic, whether intended or not, such as traumatic intrapersonal (with self) or interpersonal (with others) experiences.
In this article, we’re referring to therapeutic use and guided administration by trained professionals. Unlike recreational experiences, therapeutic psilocybin journeys include dedicated preparation, navigation, and integration support, helping ensure psychological and physical safety at every step of the way.
Understanding the Multiple Sides of Depression
Depression can come as a result of many different factors. While some people’s depression may be rooted in childhood trauma, others’ may be the result of biological imbalances or sociocultural influences.
It’s vital to recognize this complexity when aiming to treat depression, and to understand why many traditional approaches fall short.
Psychological Factors
Many people who suffer from depression experienced early-life trauma, or Adverse Childhood Experiences (ACEs), such as abuse, neglect, or loss. Studies show that going through this kind of trauma increases the chances of developing depression later in life, as it can disrupt emotional development and lead to unhealthy coping mechanisms (Madigan et al., 2023).
Trauma fosters negative core beliefs about the self and the world, which then can manifest in rumination, persistent inner criticism, emotional suppression, and social withdrawal – all typical depressive symptoms.
Processing and healing early-life trauma can significantly help relieve depression by attacking the root cause of the individual’s psychological struggles, instead of just treating the symptoms.
Sociocultural Factors
Depression may also emerge as a result of intergenerational and societal influences. It is well recognized that people exposed to unfavourable social circumstances (Kirkbride et al., 2024) are more likely to experience mental health challenges in their lifetimes.
For example, research in fields such as epigenetics (Yehuda & Lehrner, 2018) and family systems (Reese et al., 2022) suggests that trauma can be passed on across generations, perpetuating cycles of family dysfunction and vulnerability to depression.
The individualistic structures of modern society also contribute to higher rates of depression. More people than ever are experiencing loneliness and social isolation, both of which are risk factors for depression (Luo, 2022).
Many people develop depression as a result of high-stress external circumstances, such as war (Chudzicka-Czupała et al., 2023), pandemics (Pfefferbaum & North, 20202), economic uncertainty (Sarı et al., 2024), political volatility (El Khoury-Malhame et al., 2024), or discrimination. These large-scale stressors can lead to psychological distress and increased depression rates.
Biological Factors
There are also several biological reasons that a person may experience depression.
Depression is associated with reduced neuroplasticity in the brain (Rădulescu et al., 2021). Neuroplasticity is essentially the brain’s ability to adapt and reorganize based on new inputs and processes. For individuals with depression, reduced neuroplasticity means it’s more challenging to break free from rigid thought patterns and emotional responses. This also prevents the creation of new, healthy patterns of thinking and behavior.
Researchers have also witnessed elevated markers of neuroinflammation in depressed individuals (Han & Ham, 2021). This can disrupt normal brain chemistry and the function of neurotransmitters, like serotonin and dopamine, which play a key role in mood regulation (Miller & Raison, 2015).
While it’s been previously widely believed that low serotonin activity is implicated in depression, studies show that this relationship is more complex, and not simply a case of the chemical imbalance inducing depression (Moncrieff et al., 2022).
In fact, many patients don’t respond to serotonin-targeting drugs, and some exhibit normal or elevated serotonin levels.
Current research is navigating a “chicken and egg” problem when it comes to the bidirectional relationships involved in depression. The psychological, sociocultural, and biological factors described above are deeply intertwined. For example, trauma can adversely alter brain structure and function, which in turn affects cognition and emotion. Social isolation can increase brain inflammation (Finley & Schaefer, 2023) and worsen depressive symptoms (Slavich & Irwin, 2014).
These factors then reinforce each other, and it becomes difficult to define which one is the “cause” and which is the “effect.” The self-perpetuating cycles make depression difficult to treat with one-dimensional approaches.
Here’s where psilocybin comes in. The psychedelic essentially acts as a “circuit breaker”, temporarily disrupting rigid brain network activity associated with rumination and self-focus.
Guided psilocybin therapy experiences offer a holistic approach, targeting biological, psychological, and social factors and enabling individuals to break free from the entrenched loops that sustain their depression.
How Psilocybin Works in the Brain and How This Targets Depression
Understanding how psilocybin affects the brain helps explain why it shows such promise in treating depression, especially in cases that haven’t responded to conventional treatment like SSRIs.
As we mentioned above, psilocybin disrupts the default mode network (DMN), which is hyperactive in depression, helping to interrupt pathological thought patterns and rumination cycles (e.g., “I’m worthless” or “Nothing will ever change”).
This quietening of the DMN allows individuals to experience a sense of connection beyond the familiar self and access new ways of thinking that were previously inaccessible.
Psilocybin also promotes global brain connectivity, which is when regions of the brain that don’t usually “talk” to each other can communicate freely. This neural flexibility creates new insights and allows the brain to “reboot” its activity patterns.
Functional MRI scans show that after psilocybin administration, the brain shifts into a more fluid and integrated state (Daws et al., 2022), where thoughts, emotions, and perspectives have settled into a new configuration.
Another way that psilocybin works in the brain is by enhancing neuroplasticity and synaptogenesis. These two processes work in tandem, where the brain’s increased ability to reorganize itself, enabled by neuroplasticity, is facilitated by the promotion of new neural connections, which is enforced through synaptogenesis. This rewiring process is what changes the neurological underpinnings of depression, which is enabled by psilocin and the experiential effects it produces.
Michael Pollan, the author How To Change Your Mind, described this experience as “shaking the snow globe” of the mind, referring to the brain's ability to form new neural connections, essentially rewiring itself.
Research shows that a single dose of psilocybin promotes rapid neuroplasticity, with various effects lasting for days, weeks, and even months following the administration (Calder & Hasler, 2022). This is often referred to as the “critical period” within which the brain can form new connections, and patients can implement new habits and engage in social learning.
Psilocybin also catalyzes healing by amplifying emotional awareness, which can induce catharsis during the administration session. This can mean that negative beliefs and perceptions, repressed memories, unresolved grief, or existential fears come to the surface, allowing them to be processed and healed.
Many people describe processing long-held traumas and feeling self-compassion, grief, or forgiveness for the first time. Studies suggest that the intensity of the mystical or emotional experience during a guided psilocybin journey correlates with positive treatment outcomes for depression, highlighting the importance of these emotional and spiritual breakthrough moments (Brudner et al., 2025).
The Role of the Psychedelic Experience in Treating Depression
With psilocybin showing such immediate influence on brain activity, many have asked whether they can still receive therapeutic benefits without the psychedelic experience.
In other words, “Do I have to ‘trip' to experience psilocybin’s antidepressant effects?”
Research suggests that the psychedelic effects play an essential role (Yaden & Griffiths, 2020).
While studies in mice show that there are some antidepressant effects without the full “trip”, data are lacking on how this would work for humans (Hesselgrave et al., 2021).
Research on the acute effects of psilocybin—in particular, the mystical experience, ego dissolution, and emotional breakthroughs that people can experience—shows them to be important for achieving mental health improvements.
In one study on major depressive disorder, the “mystical experience” and “ego dissolution” felt during the psilocybin session were uniquely linked to how much a person’s depression improved after treatment (Weiss et al., 2024). This paper also found that psilocybin-induced mystical experience has been associated with an improvement in life quality, meaning in life, and mood in people struggling with anxiety and depression (McCulloch et al., 2022).
Research also shows that emotional breakthrough is a crucial part of the acute psychedelic experience and a key mediator in long-term psychological improvements (Roseman et al., 2019). While mystical experiences are impactful, studies indicate that psychological insights and emotional breakthroughs may be just as, or more, important for achieving positive mental health changes (Kangaslampi, 2023).
The psychedelic effects are also crucial for those working through past traumas. Trauma happens as a felt experience, and we often need a new experience to develop different responses or rewrite trauma patterns. The emotional catharsis, somatic release, and cognitive reframing that happen during psilocybin therapy sessions can support trauma release and processing.
Psychedelic journeys may also bring up forgotten or repressed memories, allowing the person to become aware and reconcile these memories. Research has shown that an important part of healing in psychedelic therapy is “re-narrating one’s own identity and biographical circumstances” after recovering unresolved traumatic memories (Rose, 2024). We’ll dive into how this works with psilocybin a little later.
What is a Psilocybin Experience Like for Treating Depression?
Depression is often rooted in unresolved psychological challenges, such as trauma, shame, self-blame, or grief. When unaddressed, these feelings can solidify into persistent negative beliefs and mood states.
Here’s where psilocybin can be especially powerful. Research and first-person reports consistently show that the psilocybin experience often induces deep emotional catharsis, or the intense release of suppressed feelings (Griffiths et al., 2016). This is often framed as “purging” or “letting go” of old pain, grief, or shame, and works not only on the level of the psyche, but also somatically, i.e., in the body.
During the psilocybin session, these effects can manifest as crying, shaking, laughing, or even yawning. It’s all normal and part of the process of mental, emotional, and physical release.
As mentioned in the previous section, psilocybin can also bring up repressed memories that have been relegated to the unconscious mind as a protective mechanism. But these memories don’t just disappear – they can manifest as depression, anxiety, or emotional numbness over time.
Psilocybin lowers these internal barriers, bringing memories to the surface in the form of visions, feelings, unfamiliar thoughts, and somatic releases. This phenomenon has even been shown in brain imaging studies.
However, it’s difficult to know whether memories that arise during psychedelic experiences are true repressed events or emerge as metaphors or constructed images (Otgaar et al., 2019). Fortunately, skilled facilitators and integration providers are trained to contextualize these experiences, focusing less on literal accuracy and more on the emotional truth and meaning for the individual.
At the core of psilocybin healing is providing a safe container for the person to explore their inner world, before, during, and after the experience. Part of this involves the set and setting during the journey – the psychological preparedness and mood state going into the session, the physical environment, and the safety and compassion felt in the relationship between journeyer and facilitator.
Another key component is the support that the person receives before and after their experience. Dedicated group or one-on-one preparation support can help an individual clarify their intentions for the journey and gain tools to navigate the challenging aspects of being in an altered state. Once they emerge from the experience, integration sessions can help them make sense of what happened and apply those insights to their everyday life.
Clinical trial protocols have found that therapeutic support before and after psilocybin experiences is vital not only for psychological safety during the session, but also in receiving mental health benefits long after it finishes (Gukasyan et al., 2022).
Is Psilocybin Safe for People with Depression?
Psilocybin has been shown to help those with major depressive disorder, treatment-resistant depression, or more minor forms of depressive disorders.
But you may be wondering, is psilocybin safe for everyone with depression?
When administered in safe environments with skilled practitioners, psilocybin has an excellent safety profile (Gukasyan et al., 2022). There is no known legal dose in humans, in stark contrast to many common medications and recreational substances.
Adverse effects during the acute experience, such as nausea, anxiety, headache, dizziness, or vomiting, are transitory and usually resolve within a day. These symptoms are best seen as part of the working-through process rather than “side effects” to mitigate.
There are, however, individuals who shouldn’t use psychedelics (Johnson et al., 2008). Those with a personal or family history of psychotic disorders (such as schizophrenia or bipolar disorder) are more likely to have a destabilizing experience.
Psilocybin is also not a replacement for emergency care in the case of active suicidal ideation. Ketamine is a better alternative in these scenarios due to its reliable, quick-acting effects (Pan et al., 2023).
Any psilocybin practitioners must conduct a thorough intake to understand the full psychological history of their participants and screen out vulnerable candidates.
Long-term adverse outcomes from psilocybin most often happen as a result of unsupervised, mismanaged, or recreational use, not from therapeutic settings. While there will always be some inherent risk to high-dose psychedelic journeys, this is remarkably low when expert care is present, such as in psilocybin therapy sessions with trained, experienced mental health practitioners.
Psychedelic Integration for Depression Turns Insight into Long-Term Change
Psychedelic integration is the process of integrating the psychedelic experience into your everyday life (Bathje et al., 2022). Psilocybin catalyzes altered states that individuals need to reflect on, process, and apply in the aftermath of the experience—this is the integration period.
The first part of integration is understanding your experience and its meaning for your healing journey. This might look like unpacking your experience verbally with a therapist or coach, or in an integration circle. By giving words to the experience, people are often able to draw more meaning from it and deepen their understanding of what came up.
Then, with this information in hand, you can transform it into action. For example, a person who connects with a sense of profound self-love and self-worth during their psilocybin session might decide to take better care of themselves by nourishing their body with healthy foods or introducing a mindful movement practice into their daily routine.
While integration absolutely can (and usually does) involve lifestyle changes, it’s not simply a to-do list of implementing new practices—it’s a process of embodiment, transformation, and perspective change that takes place on the levels of the mind, body, and spirit. Ongoing conscious behavioral change, mindfulness, specialized integration support, and somatic practices can help deepen and ground the experience into your everyday life with time.
For individuals with depression, proper integration can make the difference between a short-term reduction in symptoms and concrete, long-term positive changes. While the days and weeks post-psilocybin bring a window of neuroplasticity and “afterglow”, this wears off—and it’s the work the individual puts in to apply the lessons of their experience that will create lasting change.
Why Psilocybin Retreat Settings May Enhance Healing
When it comes to psilocybin journeying, there are generally two options that offer a safe, supportive experience: a one-on-one guided session or a retreat setting.
While many people have seen powerful results from clinical approaches, group retreat settings bring additional, profound benefits.
Nature Connection
Many retreats are set in natural environments, which are effective in helping reduce depression and provide a welcome break from overstimulating urban settings (Balanzá-Martínez & Cervera-Martínez, 2022). This connection to nature during a retreat supports nervous system regulation and can deepen the healing that takes place (Gladwell et al., 2012).
Multi-Day Immersive Format
Retreat settings offer a focused, extended setting for healing. Over several days, participants step away from everyday distractions and immerse themselves fully in the therapeutic process, while multiple psilocybin sessions allow for deeper emotional exploration. This extended arc supports a transformational journey, often likened to a “Hero’s Journey”, where individuals confront inner challenges and emerge with renewed clarity, strength, and purpose.
Group Support
Psilocybin healing is deep work, and we’re not meant to go through it alone. The group dynamics during retreats create a safe, supportive container, allowing participants to connect with and learn from each other both organically and during facilitated sharing circles. Social connection is invaluable for many people struggling with depressive symptoms, and going through a challenging experience together can help them form deep, social bonds and find relief from the isolation that often accompanies depression (Wickramaratne et al., 2022).
The research supports the value of retreat settings for psychedelic healing, too. In one study, a group of adults who were mistreated as children experienced a reduction in trauma symptoms and trait shame after taking psychedelics in an intentional group setting (Healy et al., 2025).
Another study on veterans found that psilocybin and ayahuasca retreats resulted in significant improvements to their mental well-being, quality of life, PTSD, anxiety, and depression (Calnan et al., 2025).
Where and How Can You Receive Legal Psilocybin Treatment for Depression?
Psilocybin access worldwide continues to evolve, with a patchwork of legal frameworks shaping therapeutic availability. Here’s an overview of where and how you can receive psilocybin treatment.
Legal psychedelic retreats in Jamaica and the Netherlands
Both Jamaica and the Netherlands are popular destinations for psilocybin retreats. In Jamaica, there are no laws specifically outlawing psilocybin mushrooms, making them legal for cultivation, sale, and consumption.
The Netherlands allows the sale and supervised consumption of psilocybin truffles (which are the sclerotia from certain mushroom species) while prohibiting psilocybin mushrooms themselves.
Retreat centers in both Jamaica and the Netherlands offer guided experiences in a legal, controlled environment, attracting international visitors who are unable to access the therapy in their home state or country.
Psilocybin for Depression in the USA
In the US states of Oregon and Colorado, residents can access guided psilocybin therapy through legal frameworks.
Oregon became the first state to launch regulated psilocybin services in 2023, and as of 2025, dozens of licensed service centers operate statewide. Adults over the age of 21 can access psilocybin in supervised, non-medical settings, with trained facilitators providing preparation, oversight, and integration support.
Colorado also legalized psilocybin and other plant-based psychedelics for supervised adult use. Both clinical and non-clinical trained facilitators can now provide psilocybin therapy in licensed healing centers across the state.
Accessing Psilocybin Therapy for Depression in Canada
In Canada, patients with serious or life-threatening conditions can apply for access to psilocybin therapy through Section 56 exemptions. The Special Access Program also allows healthcare providers to request psilocybin for patients suffering from conditions not manageable with conventional treatments.
However, access hasn’t been easy for many of the Canadians seeking psilocybin treatment through this program, with some patients suing the government over delayed access.
Limitations of Underground Therapy
In countries or states where psilocybin remains illegal, many individuals seek out underground practitioners. While some underground facilitators can provide skilled support, the lack of regulation introduces risks.
There’s no way to verify facilitator expertise, and often, there’s insufficient screening and psychological support, as well as no legal recourse in case harm is caused. Without the oversight of an above-ground model, preparation, facilitation, and integration standards vary widely, heightening the risk of adverse or traumatic outcomes.
Meanwhile, legal, regulated centers provide medical and psychological screening, professional facilitators, accurate dosing, and structured integration—factors proven to increase the safety and effectiveness of psilocybin therapy.
There’s also no legal risk for pursuing healing when taking the regulated route. This peace of mind is essential for undertaking meaningful therapeutic work.
Why Choose MycoMeditations to Treat Depression with Psilocybin Therapy?
If you’re seeking psilocybin treatment for depression, a MycoMeditations psilocybin retreat might be just what you’re looking for.
Our unique approach is designed to help you achieve lasting mental health improvements, combining traditional knowledge with cutting-edge research and evidence-based therapeutic modalities. MycoMeditations is designed to be the most therapeutically rigorous psychedelic retreat in the world.
Experienced licensed therapists and facilitators accompany you to ensure you feel safe and supported from the moment you sign up. We provide individualized care throughout the retreat and follow-up, structured integration sessions so you can maximize your chances of creating real, lasting change and finding relief from depression.
The data we have gathered over multiple years has shown that the MycoMeditations psilocybin-assisted retreat model provides comparable positive treatment outcomes for depression as shown in clinical trials, with clinically significant improvements in depression maintained one year after the retreat.
Curious about what our guests have to say? Read about their experiences on our testimonials page.
Psilocybin and the Path Forward into a New Depression Treatment
As we’ve explored throughout this guide, the science behind psilocybin is robust, evolving, and remarkably promising.
Clinical trials, brain imaging studies, and firsthand accounts all point to the same conclusion: psilocybin, when administered with care and paired with therapeutic support, has the potential to bring deep, lasting relief to those suffering from depression.
At its core, psilocybin therapy extends beyond the realm of biochemistry and brain scans. It’s about transformation. Psilocybin helps individuals to reconnect with their emotions, rewrite painful narratives, and release what no longer serves them, so they can break free from depression and cultivate a life of joy and purpose.
We are in the midst of a renaissance in mental health care—one that embraces holistic approaches to healing and the wisdom of altered states. We genuinely believe that psilocybin is at the center of this movement, not as a miracle cure, but as a powerful catalyst for change when used with intention, safety, and integration.
Psilocybin represents a turning point for so many struggling with debilitating mental health symptoms—a return to a sense of wholeness and hope.
If you’re struggling with depression and are curious whether a psilocybin-assisted retreat might be right for you, explore our programs at MycoMeditations.